Ventilation is controlled by both peripheral (which responds primarily to falls in PaO2) and central chemoreceptors (which respond to a rise in PaCO2). However, the primary drive to breath comes from the hydrogen ion concentration (and hence PaCO2) in interstitial fluid in the brain surrounding the central chemoreceptors (CSF).
The partial pressure of arterial oxygen at which ventilation increases significantly is 60mmHg (this is the partial pressure or arterial oxygen at which haemoglobin will start to desaturate, i.e., the where the oxyhaemoglobin dissociation curve starts to fall).
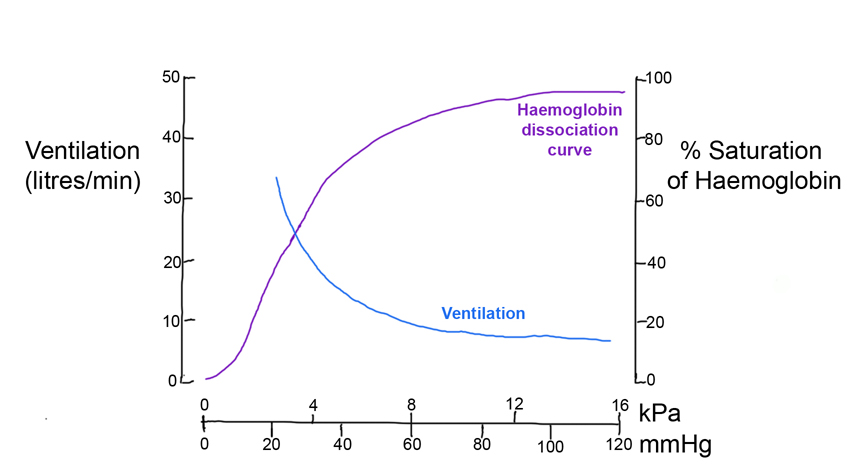
However, the corresponding curve for carbon dioxide is more linear.
Thus ventilation is more tightly controlled around PaCO2 (i.e., any change in PaCO2 will immediately change ventilation). The reason for this is that changes in PaCO2 will change arterial pH and this will have various physiological effects, e.g., changes in membrane excitability and enzyme function. However the rise in ventilation in response to a rise in PaCO2 is magnified if PaO2 is also lowered.
As Mr Guzdeck has COPD, he is probably always a little hypoxic and has chronic CO2 retention. The pH of his CSF has thus had time to return to near normal levels and his central chemoreceptor drive from hydrogen ions is almost abolished. Thus, his ventilatory drive is now primarily from stimulation of the peripheral chemoreceptors by the low PaO2. By increasing the patients PaO2 you will reduce his drive to breathe.
.